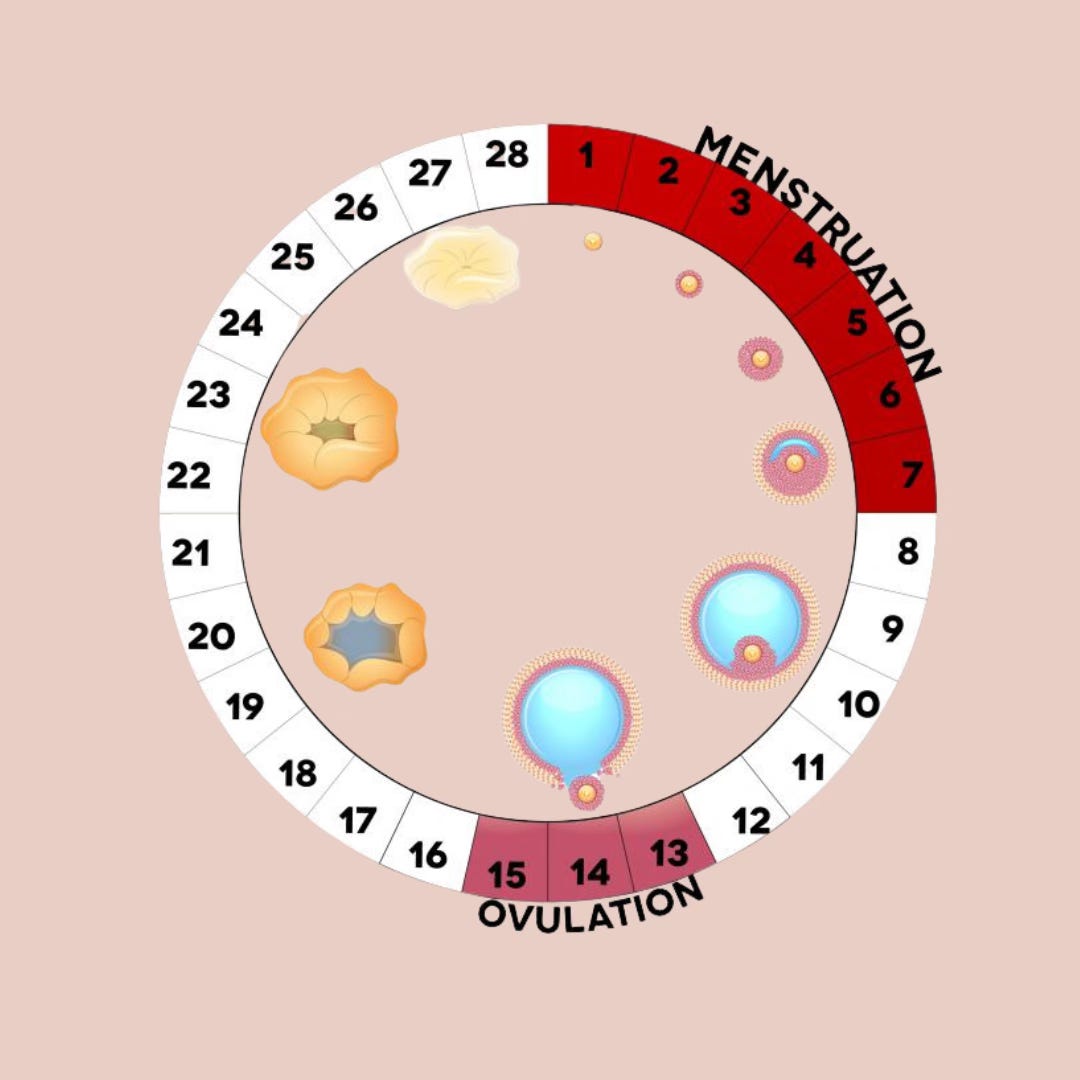
In our last newsletter, we explored the main event of the cycle—ovulation. Today, we're diving into the key signs that may indicate you're not ovulating and the potential reasons why.
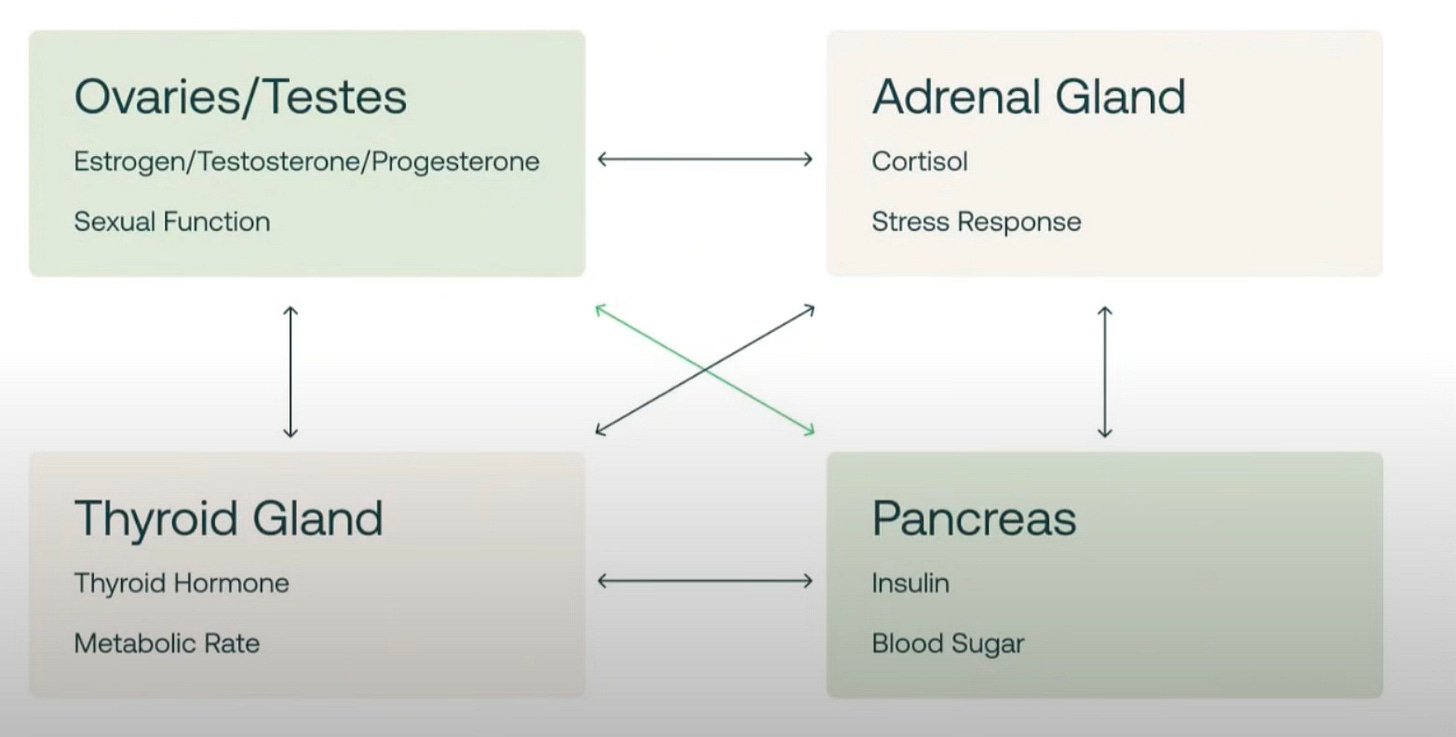
Hormones are like a symphony. When one instrument is off-key, it disrupts the harmony of the entire orchestra. Ovulation depends on precise communication between the brain, ovaries, adrenals, and thyroid—hundreds of hormonal signals influence this one critical event.
Ovulatory disorders are a leading cause of female infertility. Experiencing anovulation doesn’t mean you’ll never ovulate again, but it's essential to identify and address the root causes.
Since ovulation is considered a fifth vital sign of health for women [1], how can you be sure it's happening? Fertility awareness methods (FAM) empower women to track biomarkers that confirm ovulation. But if ovulation isn’t happening, here are key signs to look for.
🚩 Signs You May Not Be Ovulating
Missing or Irregular Periods
Ovulation drives the cycle’s rhythm. Irregular or absent periods often signal an ovulatory disorder or lack of ovulation.Limited or No Cervical Mucus
Estrogen prompts the cervix to produce fertile (egg-white) mucus leading up to ovulation. Little to no mucus could indicate low estrogen or absent ovulation. Factors like stress, allergy meds, diet, and exercise can also affect mucus production.
👉 [Check out this resource to learn more about cervical mucus.]No Temperature Increase
A slight rise in basal body temperature (BBT) after ovulation confirms that it occurred. Flat or erratic BBT patterns can signal anovulation.Abnormal Bleeding
Spotting or irregular bleeding between periods can be a sign of hormonal imbalance impacting ovulation.
❓ Why Ovulation May Not Be Occurring
1. Glucose / Insulin Dysregulation
Unstable blood sugar levels can lead to insulin resistance, affecting ovarian function. High insulin levels can increase androgen production, which inhibits ovulation—a common issue in PCOS.
According to the NIDDK, over 1 in 3 U.S. adults aged 18+ had prediabetes in 2021 [2].
Surprisingly, about 40% of American adults aged 18-44 without diabetes still have insulin resistance, and nearly half of them aren’t classified as obese by BMI [3]. Glucose dysregulation could be a hidden culprit behind hormonal dysfunction.
Interestingly, our bodies process carbs differently depending on the cycle phase.
Research using continuous glucose monitors (CGM) shows that glucose peaks during the luteal phase and is lowest in the late-follicular phase. This is why cravings and mood swings tend to spike during the luteal phase. [4]
🔄 Cycle-syncing your diet can be a game-changer. [Check out the cycle-syncing recipe book on the RoseFem resource page.]
Curious if blood sugar is impacting your hormones? Consider consulting a practitioner who utilizes CGMs.
2. Chronic Stress
Chronic stress is one of the most common disruptors of hormonal balance. Elevated cortisol levels can suppress GnRH, FSH, and LH—essential hormones for ovulation.
Common signs of cortisol imbalance:
Feeling "wired and tired" (awake at night, sluggish in the morning)
Consistently waking between 3-4 AM
Weight gain, as the body holds onto fat in survival mode
If this sounds familiar, it’s worth exploring stress-reducing strategies like building a better sleep routine, light exercise, prayer, and spending more time in nature.
3. Undernourishment / Over-Exercising
Low caloric intake or excessive exercise can trigger survival stress, reducing GnRH and halting ovulation. This can lead to hypothalamic amenorrhea.
As a former college athlete, I know the temptation to ignore absent periods—but it’s a sign your body needs support, not more pressure.
4. Nutrient Deficiency
Protein is foundational for hormone health, with many nutritionists recommending 25-30g of protein per meal and up to 1g per pound of lean body mass.
But while protein and healthy fats are essential, key micronutrients are equally crucial. Vitamins and minerals like Vitamin D, B6, B12, zinc, iron, selenium, and magnesium play vital roles in ovulation.
Focus on whole-food protein sources and quality nutrients. Remember, we can be overfed but undernourished.
👉 For a comprehensive nutrition guide, I recommend the book Real Food for Fertility.
5. Hormonal Imbalances
Low Estrogen & Progesterone: Low estrogen can prevent follicle development. Low progesterone after ovulation can suggest inadequate ovulation.
Thyroid Issues: Conditions like hypothyroidism can slow metabolism and disrupt hormone production.
High Prolactin Levels: Elevated prolactin can suppress ovulation.
6. Hormonal Contraception
Hormonal birth control (pill, patch, IUD) suppresses ovulation by blocking natural hormone fluctuations. Without these natural rhythms, ovulation doesn’t occur.
If you’ve recently stopped birth control, it can take months for cycles to normalize. Your body may need time to detox and replenish nutrients. More on post-birth control syndrome in a future post!
💡 When to Seek Support
Does this sound like you?
You're experiencing one or more signs of anovulation.
You want to come off hormonal birth control.
You need nutrition guidance for fertility-supportive eating.
You’re curious about cycle-syncing your nutrition, mindset, and movement.
You’re seeking a specialist to uncover the root of hormonal imbalances—RoseFem’s referral network can assist.
✨ Take the next step toward integrated hormone wellness with a free 15-minute hormone consult.
Understand your body. Become a genius of your hormones. Flourish in your femininity.
And as a final note of encouragement: go on a quest for beauty this spring—time outside is one of the best things you can do for your hormones! 🌿